The Menopause Conversation We Should All Be Having
And how to show up for the women around you.

Welcome to Truth Be Told, the weekly food and fitness newsletter published by The Whole Truth Foods.
Editor’s note: A constant thread in conversations around gender is responsibility. When everyday behaviours stem from misunderstanding biological realities, whose job is it to bridge that gap? Should women explain what's happening to them, or should everyone else take ownership and learn?
You know our answer at TBT. It's the latter. Which is why we publish stories that unveil the invisible layers behind cultural attitudes.
Aruna Chawla's piece today tackles one of those casually ignored issues: menopause. It's as natural as ageing itself, but if we don't understand it, how can we support the women around us? Let this piece be your starting point.
Aruna Chawla is a writer, researcher, and trained lawyer examining the business, policy, and power structures of health, with a focus on female healthcare and systemic access to wellness and safety. You can reach her at @arunachawla_ on Instagram and Twitter.
PS: Here is a short feedback form to help us understand how we're doing. Would you please share your thoughts? Link here. For more, you’ve got my email.
— Samarth Bansal (samarth@thewholetruthfoods.com)
Maya is 45. She's the kind of person whose energy fills a room before she even speaks. A mother of two, an executive at work, a spreadsheet-and-birthday-cake kind of woman. The one who remembers your dentist appointment and your blood test.
But lately, something’s changed.
She forgets words mid-sentence. She’s exhausted after doing nothing. She wakes up drenched in sweat. Her family says she’s snapping more. Her colleagues say she’s distracted, and maybe her time is up. She just feels… not like herself.
She suspects it could be menopause—the biological transition when a woman’s ovaries stop releasing eggs and her periods end permanently. But without clear guidance, she's not sure what to expect or how to ask for help. When she brings up her symptoms, they’re brushed off.
"Maybe you’re stressed." (Who isn’t?)
"It’s just hormones." (Yes, and?)
"Try some yoga." (Oh wow, why didn’t I think of it before!)
This is what perimenopause can look like, even when no one calls it that. This is the years-long transition leading up to menopause when hormone levels fluctuate wildly, causing unpredictable symptoms before periods stop altogether.
This is why we need a better script. One that explains what’s happening and how to show up for the women in your life who are going through it. This guide is written for you, whether you're a partner, child, or colleague, because support starts with understanding.
I. What Menopause Actually Is
Let’s start here: menopause is not a disease. It’s not a breakdown. It’s not a crisis.
Menopause is an outcome of ovarian ageing, a biological transition that marks the end of ovulation and menstruation in female bodies. It is officially diagnosed after 12 months of a woman not experiencing menstruation. But the transition starts years earlier, in perimenopause, when estrogen levels start to fluctuate, triggering a wave of physical and cognitive changes.
And because estrogen influences nearly every major system in the body—brain, bones, heart, skin, sleep, mood—its decline brings wide-ranging effects.
One way to understand menopause is to think of it as ‘puberty in reverse’. The body's hormonal cycle is recalibrating for a post-reproductive life. And because we don’t have enough institutional or cultural support to navigate this change, symptoms often feel overwhelming.
So yes, it is hormonal. But that doesn’t mean it’s minor.
Hormones aren’t feelings. They are infrastructure. They are the signal system that keeps your body and mind in sync. When they shift, everything does.
But we’ve turned “hormonal” into a synonym for irrational, as if it’s an insult. As if only women have hormones, and only female hormones change (which they do at a higher rate than males’, but all humans have hormones that go through their changes!).
This is why someone like Maya might feel like she’s changing in ways she can’t predict, name, or control.
That’s a problem. Because it stops us from recognising the very real and systemic nature of this transition.
II. What the Menopause Transition Feels Like
Maya’s symptoms didn’t come all at once. First came the sleepless nights. Then the forgetfulness. Then the sudden waves of heat that made her feel like her body was on fire. They disrupt identity, productivity, and relationships.
Here’s what she, and many others, might be experiencing:
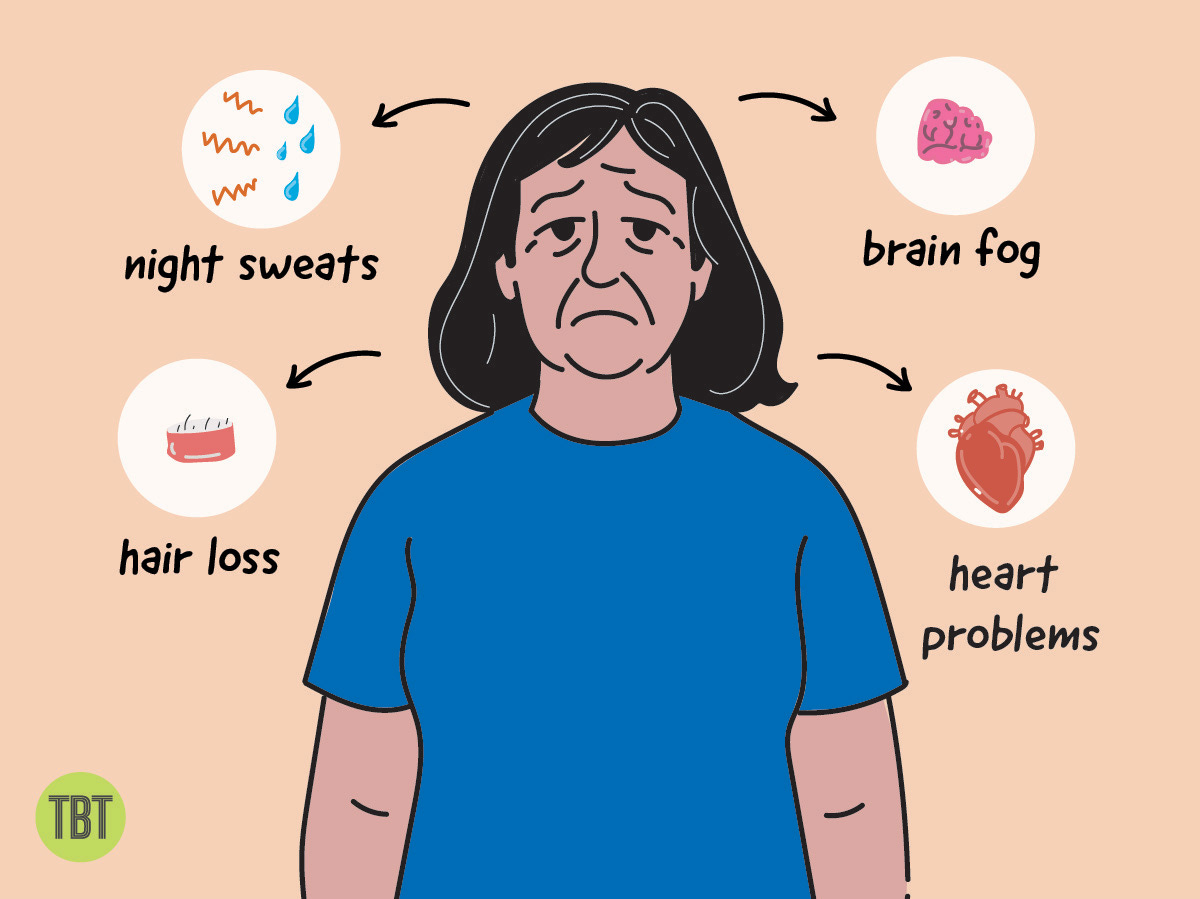
1. Hot Flashes & Night Sweats: Sudden waves of heat, sweating, and discomfort, often followed by poor sleep, fatigue, and insomnia. Estrogen fluctuation affects the body’s temperature regulation.
2. Brain Fog: Memory lapses, mental fatigue, and trouble with focus. These can interfere with work, confidence, and decision-making.
3. Metabolic Changes: Increased abdominal fat, glucose dysregulation, and higher cardiovascular risk. These are not just aesthetic issues but also affect long-term health outcomes.
4. Hair Loss: Thinning hair, linked to stress, hormonal shifts, and poor sleep. It’s not just cosmetic. It's a visible sign of systemic strain.
These symptoms are not "in her head." They are biological shifts in need of real-world support.
III. A Rare Evolutionary Transition
Here’s something you probably didn’t learn in biology class: menopause is biologically rare.
Most female mammals continue reproducing until they die, or only live a short time beyond their last pregnancy. Human women are different. We can live 30–40 years beyond our reproductive years. This longevity is an evolutionary opportunity that humans have unlocked.
Only a handful of species on Earth share this trait: humans, orcas, beluga whales, narwhals, and pilot whales. In each of them, older females play outsized roles in the survival of their communities.
Take orcas. Scientists studying pods off the Pacific Northwest coast found that post-reproductive female orcas guide younger whales to food sources and protect their sons from conflict. In humans, we see echoes of this in what’s called the grandmother hypothesis, the idea that women evolved to live longer to support their children and grandchildren, helping families thrive across generations.
In other words, menopause isn’t a glitch. It’s a feature. A signal that a woman’s role in her community is shifting, not ending.
And yet, culturally, we treat it as a decline. As if a woman’s worth drops the moment her periods stop. As if no longer menstruating means no longer mattering.
So if menopause is this rare evolutionary advantage, why do we struggle so much to talk about it?
IV. Why Don’t We Talk About It?
Because we don’t know how.
We teach girls what to expect from puberty. We throw parties for baby bumps. But when it comes to menopause, a transition just as inevitable, we go silent. Or worse, we dismiss it with a shrug and a joke.
Indian women, on average, hit menopause at 46.6 years, which is earlier than in many countries. A mix of early marriage and childbirth, chronic nutritional deficiencies, reproductive conditions like PCOS, and relentless environmental stress all play a role.
At this age, many women are still parenting, caregiving, or leading teams. They’re in the middle of everything, and yet still left to navigate this transition without guidance.
Symptoms like Maya’s are written off. Fatigue becomes laziness. Mood swings become personality flaws. Forgetfulness becomes incompetence. And because society doesn’t name what’s happening, women often stop talking.
She might suspect it's menopause but without validation, education, or support, she’s forced to power through alone.
I’d love to see a future where we celebrate menopause (and ageing across the board). How wonderful would it be to celebrate the outsized roles older women can play in keeping our communities together with their experience, wisdom, and support!
V. How We Got the Narrative So Wrong
When women are left in the dark about their bodies, someone else always profits from the confusion.
In 1966, a book called Feminine Forever became a cultural phenomenon. Written by Dr. Robert Wilson, it claimed that menopause was uncomfortable because it was pathological. According to Wilson, women were never meant to live past menopause, and once they did, they became “flawed” and “unfeminine.”
His solution was lifelong estrogen therapy. Not for health, but for appearance. Estrogen, he argued, would keep women attractive to their husbands. (He even claimed men judged women from “the ankle up.” YUCK.)
The book sold over 100,000 copies in its first year. Why? Because no one else was talking about menopause. Wilson’s narrative was false, sexist, and shockingly reductionist. It spread quickly through both culture and medicine.
What most readers didn’t know: the book was funded by pharmaceutical companies that manufactured estrogen.
That funding trail matters. Because it illustrates what happens when silence surrounds a life stage that half the population will go through. Misinformation thrives. Industry steps in. And a natural transition gets rebranded as a deficiency.
This is where the “menopause = disease” narrative took root. Not in science. In marketing.
And it’s still with us today. You see it in how menopause is framed as “failure” or “decline.” You see it in how clinical care lags for midlife women. You see it in how we medicalise without educating, prescribe without context, and still, decades later, leave women with more questions than answers.
We need better medicine. But we also need better stories.
The way menopause is framed—a loss, a decline, an end—isn’t just inaccurate, it’s limiting. Yes, women face real physiological changes, but this isn’t just about symptoms and challenges. With the right support, this phase can be a turning point—a time to reimagine careers, priorities, and possibilities. It is a $16 billion industry and yet the focus continues to be on medicines, supplements, and what women themselves need to do, additionally, instead of creating systems that allow them to navigate this transition with the right support.
In India alone, 2.2% of women experience premature menopause, and 16.2% experience early menopause—and still, we don’t talk about it enough. Someone in your life is already going through this. The more we normalise these conversations, the less women will feel dismissed, sidelined, or patronised.
Educating yourself isn’t difficult. But it can change everything for the women around you.
VI. What Support Looks Like
When Maya started waking up drenched in sweat at 3 am, her husband suggested she drink more water. When she snapped at her teenage daughter for chewing too loudly, her colleagues joked that she was “extra sensitive these days.” When she forgot to attend a meeting she herself had scheduled, she called herself lazy and scattered.
No one, including Maya, realised that her brain, body, and emotions were recalibrating. What she needed wasn’t “more discipline” but more understanding, more data, and better care.
Here are some ideas on what you can do:
1. Stop making food a moral battleground: Women in perimenopause often struggle with blood sugar crashes and cravings because estrogen affects insulin sensitivity. Focus on nourishment over restriction. Offer to cook protein-rich meals. Don't comment on portions.
2. Be her movement partner, not her trainer: Movement is one of the most effective ways to alleviate menopausal symptoms, especially strength training, which helps protect against bone loss, insulin resistance, and muscle decline. Instead of saying "You should exercise," ask "Want to take a walk?" Offer your time, not advice.
3. Support informed medical care: Perimenopause increases the risk of insulin resistance, metabolic syndrome, and cardiovascular strain. Encourage her to check key markers: blood sugar tests (fasting insulin, glucose, A1C), lipid profile, vitamins (D and B12), and thyroid panel. If she's considering hormone therapy, help her find knowledgeable doctors but let her make the decisions.
4. Stop dismissing mood changes: Instead of labelling her emotions as irrational, ask: "How are you feeling today?" or "Would you like to talk, or do you want space?"
5. At home, shift the emotional load: Look around and ask: What do you assume she'll handle? Where can you step up without being asked?
6. At work, make space without making it awkward: Don't joke about forgetfulness. Normalise temperature control and quiet zones. If you're a manager, make it safe to name the phase.
In short, if you're a partner, child, or colleague, your role isn't to solve menopause. It's to stop pretending it doesn't matter. Because how you show up now will shape what midlife feels like for the women in your life. And for every generation that follows.









Lovely article - what was extra special is the "to-do's" which were connecting and illuminating, for many times we know we are wrong, we just do not know the steps to correct the same. Thank you. and glad i am a part of this newsletter.
One of the best written articles I have read. Very informative, structured and practical